As the world looks to find new ways to battle disease from viruses and bacteria, a common metal that mankind has been mining and producing for millennia has shown remarkable abilities in this struggle. That common item is copper, which has both antibacterial and antiviral properties and is capable of killing both within hours of contact. Interestingly, the realization of copper’s benefits in medicine are not new. The first documented use of Copper to fight disease appeared in books written in ancient Egypt between 2600 – 2200 B.C., describing its use to fight infections in wounds and to sterilize drinking water. Similar writings are also found in the history of Greeks, Romans, Aztecs, Hindus and Persians (1).
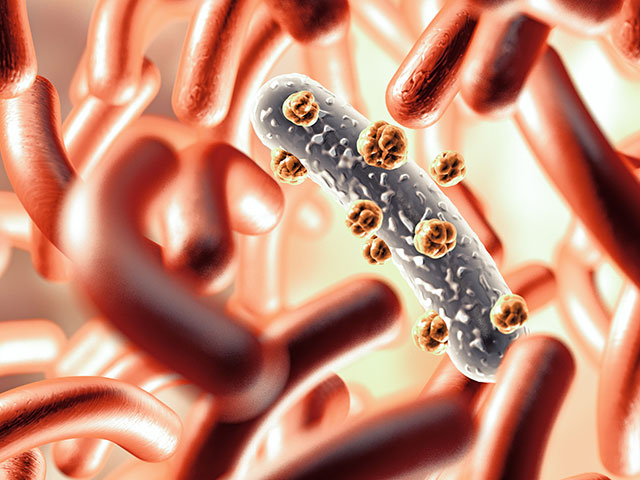
It is however only recently been discovered how copper actually works to prevent disease. The answer is in the release of electrically charged ion particles when a virus or microbe lands on the surface of copper. The released ions proceed to prevent cells from creating energy from sugars, punch holes in the bacterial cell membrane or break down the coating on a virus, and then destroy the DNA and RNA inside the cell (2).
In the fight against COVID-19, a recent study by the CDC found that the virus was no longer viable after 4 hours on the surface of copper, versus 1 – 3 days on the surface of cardboard, stainless steel and plastics (3). The promise of these results are very positive for the use of copper in public and medical settings and once again show its incredible properties in the fight against disease.
- Dollwet, H.H.A. & Sorenson, J.R.J.. (1985). Historic uses of copper compounds in medicine. Trace Elements in Medicine. 2. 80-87.
- Warnes SL(1), Caves V, Keevil CW. (Epub 2011 Dec 19) Mechanism of copper surface toxicity in Escherichia coli O157:H7 and Salmonella involves immediate membrane depolarization followed by slower rate of DNA destruction which differs from that observed for Gram-positive bacteria. Environmental Healthcare Unit, University of Southampton, Highfield, Southampton, UK.
- N Engl J Med 2020; 382:1564-1567 DOI: 10.1056/NEJMc2004973